Day 1: How My Doctor Missed My Breast Cancer Symptoms [Kristen Vengler]
![Day 1: How My Doctor Missed My Breast Cancer Symptoms [Kristen Vengler] Day 1: How My Doctor Missed My Breast Cancer Symptoms [Kristen Vengler]](https://getpodpage.com/image_transform_gate_v3/I_zHrnrEetbqB1-4Q0zqer7Mp62TFyaT53rrbnTSIS8=/?image_url=https%3A%2F%2Fd3wo5wojvuv7l.cloudfront.net%2Ft_rss_itunes_square_1400%2Fimages.spreaker.com%2Foriginal%2F3d22b544fecb7b967903f0f46823dcce.jpg&w=1200&h=630&fill=blur)
When Kristen noticed her right nipple felt different, her first thought was "what the F is this?" Her second thought was that her life was about to change. So she did what everyone does in this situation... she jumped out of the shower, went to...
When Kristen noticed her right nipple felt different, her first thought was "what the F is this?" Her second thought was that her life was about to change. So she did what everyone does in this situation... she jumped out of the shower, went to Google, and diagnosed herself with a rare form of breast cancer called Paget’s Disease.
But Google’s never right about these things, so a few days later when the radiologist suggested a biopsy for Paget’s, shit got real. Overnight, life became a tightly-woven schedule of appointments wedged between work: a biopsy, an MRI, a colonoscopy, and a million different labs and scans leading up to the first chemo treatment. As a single woman with limited resources, Kristen had no choice but to advocate for herself, quickly figuring out the magic words to use with her healthcare providers to move the process along faster and start treatment sooner. In this episode recorded on her first day of chemo,
Kristen tells us what’s happened so far, including why her mammogram didn’t catch the tumor, what made her cry and what made her throw up at the first chemo appointment, and how nearly taking her own life a year earlier prepared her to confront breast cancer with strength and courage instead of defeat. From the awful moment in the shower through the last day of radiation and beyond — this is Kristen’s breast cancer story, told in real time.
Subscribe to our newsletter here
Meet Kristen’s doctors: surgical oncologist Dr. Louis Rivera, hematologist and oncologist Dr. Sonia Ali, plastic surgeon Dr. Salvatore Pacella, and radiation oncologists Dr. Anuradha Koka and Dr. Kenneth T. Shimizu.
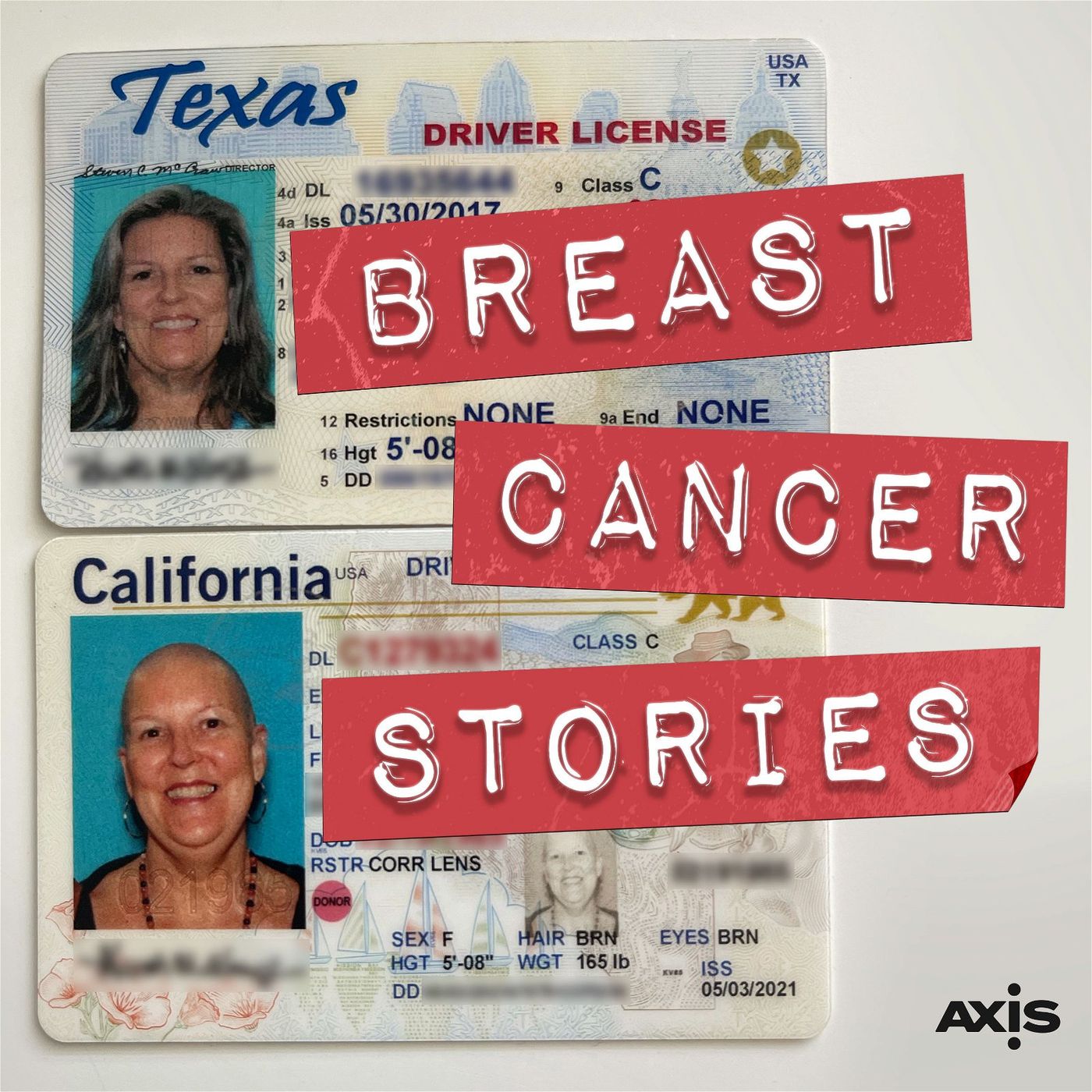
About Breast Cancer Stories
Breast Cancer Stories follows Kristen Vengler, a 56 year old single empty nester in San Diego, from her diagnosis of hormone positive breast cancer through chemotherapy, mastectomy & breast reconstruction, radiation, and whatever happens after that. In 2020, Kristen moved from Austin to San Diego to be near family and start her life over after a life-shattering workplace trauma. A few months later she had that terrifying moment in the shower we all hope we never have. From her breast cancer diagnosis, through chemotherapy, breast reconstruction, and radiation, we experience each new milestone as it happens.
This podcast is about what happens when you have breast cancer, told in real time.
Support the show by sharing online, writing a review, or donating at https://www.breastcancerstoriespodcast.com/p/donate/
Host and Executive Producer: Eva Sheie
Co-Host: Kristen Vengler
Editor and Audio Engineer: Daniel Croeser
Theme Music: Them Highs and Lows, Bird of Figment
Story Editor: Mary Ellen Clarkson
Assistant Producer: Hannah Burkhart
Cover Art Designer: Shawn Hiatt
Breast Cancer Stories is a production of The Axis.
PROUDLY MADE IN AUSTIN, TEXAS
Kristen (00:00):
That was something that, every day when I would wake up, I'd go, oh, and I'd go, oh, yeah. Shit, I have cancer, I got to deal with this.
Eva Sheie (00:11):
This is the story of my friend Kristen. Last year, Kristen moved from Austin to San Diego to be near family and start her life over, and just a few months later, she had that terrifying moment in the shower we all hope we never have. Because Kristen and I are friends and I know her life, on this podcast, we're comfortable talking about things strangers might not be. We're sharing her story, because we want others confronting this challenge to have something to lean on. This podcast is about what happens when you have breast cancer, told in real time.
Eva Sheie (00:44):
Go back to the beginning, how did this even come up? How did you figure out that you had breast cancer?
Kristen (00:56):
So, I had been out of town on a meditation retreat, and I got home, it was the Sunday before Thanksgiving. And I was taking a shower, and I noticed that my right nipple felt different than my left one when I washed it. And it felt different in that it was bigger. And it was also like more flesh to the skin, and there was a little bit of an indentation down towards the bottom, where the aerial is.
Eva Sheie (01:23):
What was your first thought?
Kristen (01:25):
Me, I was like, what the fuck is this? I looked at it, and I was like... I mean it was actually one of those few times in your life where you do a 180, and you realize, right then your life probably changed. And , so I looked at it, and I was like, huh. It was toward the bottom, so I took pictures so I could see and zoom in on exactly what it looked like.
Kristen (01:49):
And then, of course, I went to the internet, and what it said first was that it was likely something called Paget's, or Paget's disease. I don't know how they pronounce it, and that's actually a disease of the nipple, that is... Usually there's some advanced cancer that's going on when that's there, and it's a tough one. It's a rare disease. It happens, I want to say, 5% to 10%, maybe max. Could be 1% to 5%, I can't remember that exactly right now.
Kristen (02:17):
And I was like, oh God, Kristen, no, whatever. I hadn't established my primary care physicians or anything here, so, and I'm on the Scripps HMO, so I had to do that. I got a Zoom call with her, and then she wanted me to come in. And what really got people to get me in to see them is I would say, I can see and feel it. And that...they were like, oh, okay, this could be something.
Eva Sheie (02:45):
When was your last mammogram?
Kristen (02:48):
So, this mammogram was in November, I guess. November, December of this year, and right before that, it was 18 months before.
Eva Sheie (02:56):
Oh, so not that long, really.
Kristen (02:57):
No. I was really good about having them done.
Eva Sheie (03:01):
I think, what do they put us on, five years, 10 years? I don't know. I'm supposed to have one soon.
Kristen (03:07):
I think over 50 they have you do it like once a year.
Eva Sheie (03:10):
I think they just changed it to every other year.
Kristen (03:13):
Oh did they? Okay. Well, so I wasn't...it wasn't like I was that far past. It was like six months.
Eva Sheie (03:19):
It's actually pretty controversial that they reduced it from once a year to every other year.
Kristen (03:24):
Oh, is it?
Eva Sheie (03:25):
Yeah, because I think there's a lot of doctors who are angry that they won't catch as much as soon.
Kristen (03:30):
Right. Well, that's true. You know, and the thing was that when I did the mammogram this time, it caught it. But what's interesting is like I have like dense breast tissue. So the biopsy on the lymph node isn't back yet. That should be back in the next couple of days. But it's nowhere else in my breast. It's like a one inch round tumor that is right behind the nipple and areola.
Kristen (03:56):
And so that skin tends to get hard at times too, you know like when you're cold, or like whatever. It's very different tissue than like your regular breast skin. And so, you couldn't see anything from either mammogram. They were clear. And I actually had, I think the year before that, I had an ultrasound too, because it was just dense breast tissue and that kind of thing.
Eva Sheie (04:18):
So you were on top of it.
Kristen (04:19):
Yeah, totally on top of it. I mean again, I hadn't established all my stuff here since I moved 10 months before, 11 months before. But I knew I needed a mammogram and I needed a colonoscopy too. Those are things I knew I needed, and I got all that stuff done with all of this. So like my colonoscopy was scheduled for February. Then when I found out that I had breast cancer, I was like, you know what, let's just move it up, and just be sure all that's clear, too.
Kristen (04:46):
That was part of my week, last week. Let's start it off Monday with a colonoscopy. And then it was all these tests and then my port placement and labs and just like bam, bam, bam. But I'm so glad that as hard of a week as it was, and as emotional and like tiring that like, it wasn't like, okay, let's do this bone scan and wait a week. Let's do this and wait a week. It was fast and furious, but I got answers, and we know what we're looking at. So I love the information piece always. It makes me feel like I'm in control.
Eva Sheie (05:23):
How much time went by between when you found out and when all of this process of being treated started?
Kristen (05:32):
Less than a month. Well, no, just a little over a month. I found it, and it took about a week to get a Zoom meeting with my primary care, then another week or so to get in with her for her to see me, because it has to go through all these referral processes, right? And, so then she referred me for the mammogram and ultrasound, and that took another two weeks.
Kristen (05:57):
The beginning took a lot longer. And so then once I got into the mammogram, and ultrasound, the radiologist comes in, she goes, "Well, you know what we're looking at here, I think is Paget's disease." I was like, "No. Wait a minute, that's what the internet said. It's never the rare disease. Come on, come on, it has to be something else."
Eva Sheie (06:16):
Did you joke with her like that?
Kristen (06:18):
Yeah, exactly. I was like, "Are you kidding?" I'm like, "Well, no. If you put it in, that's what you're going to find, it's always a rare disease." At least it's in this country, you know, it's not like in Zimbabwe or something. But she's worried about that. So that report referred me to a surgeon and suggested an MRI. So I got in to see the surgeon pretty quickly.
Kristen (06:40):
And I was like a bulldog. When they would tell me that the MRI was two and a half weeks out, I was calling every day, the appointment place saying, "Do you have any cancellations? Do you have any cancellations?" Like I didn't want to wait. I wanted to find out what's going on.
Eva Sheie (06:55):
Smart.
Kristen (06:56):
I got in like, my MRI, I got in like a little over a week earlier. So that was the key to getting this moved up. Because he said at the MRI before he even got the biopsy back. So after the mammogram, I went to the surgeon, he did what's called a punch biopsy.
Eva Sheie (07:15):
What kind of surgeon is this?
Kristen (07:17):
Oncology surgeon. I mean like a cancer surgeon.
Eva Sheie (07:21):
Okay.
Kristen (07:22):
He is at MD Anderson.
Eva Sheie (07:23):
What's his name?
Kristen (07:25):
His name is Rivera, Dr. Rivera. Can't remember his first name. Anyhow, so he did what's called a punch biopsy, which is basically where they numb... That was painful, actually... I mean relatively, it was uncomfortable, I should say. And so he was able to punch like a two millimeter piece of skin. It was like a needle, but it had a little canister in it where they punch it.
Kristen (07:49):
And they sent that back. He did that on December the 15th, I think. Yeah, and the next Friday on the 18th he called me and said it was malignant carcinoma.
Eva Sheie (08:02):
He called you himself?
Kristen (08:04):
Yes. Oh yeah. The care that I'm getting and the personalization, and the bedside manner is like nothing I've ever seen. It's incredible.
Eva Sheie (08:13):
I'm just looking at him online. So one of my great specialties is looking up doctors online.
Kristen (08:19):
Right. Right.
Eva Sheie (08:20):
From the work that I do. And he's board certified in general surgery. So his original training was in lots of things, and then after that, he went on to specialize in removing cancer. So he knows how to do lots of stuff, but he got board certified in 2007. So he's mid-career, which means he has a lot of experience. He probably works really long hours right now.
Eva Sheie (08:46):
But I can tell by just looking at his background, that you're in really good hands because he's got good credentials, and they're hard to read, for most people, but... And he was in the Navy, so he's ex military and the surgeons who come out of the military, a lot of them land in San Diego.
Kristen (09:06):
Right, Well, it's funny, the GI doctor who did my colonoscopy, he's like, "Hey, I golf with Dr. Rivera. We were in the Navy together, he's a good guy, you're in good hands." So it's funny, you would think it's a bigger community than that, it's a pretty big city, but it's not really.
Eva Sheie (09:24):
It's not.
Kristen (09:27):
Well, so, yeah, he called me himself from his cell phone. And then, he even asked, he said, "If I get results over the weekend, can I call you this weekend?" So he really wanted to get the information quickly. And, so then they did the MRI, and the MRI confirmed what was going on. But what, also, what he did when he found that it was malignant and he sent me the report and all of that, after the fact.
Kristen (09:53):
So I think what's really cool is that in this portal, I can see all the test results, but when it's a biopsy, that could be malignant or some bad news, the doctor has to release it. So, I don't see it first, which that's key. But he referred me immediately to a radiation doctor, and also my oncologist, Dr. Ali. She's so good. A-L-I, her name is Sonia Ali. He had those appointments set up. I mean he got those referrals within minutes, and I got appointments, it was like right after Christmas.
Eva Sheie (10:31):
So she looks to be a hematologist and an oncologist. She looks very nice, you know, because you can tell good doctors by their photos. No, you can't.
Kristen (10:46):
No, but she is nice. I like her. A friend of a friend who had breast cancer, who I was talking to, she has her as well, and she just went through everything. Hers was stage one and it was a little different than mine. But she raves about her. And every time I would go and get blood drawn or an EKG for a baseline for all this, they're like, "Dr. Ali is awesome." You know, like people know her.
Eva Sheie (11:13):
You said, your friend is stage one, you're at stage three.
Kristen (11:17):
Right.
Eva Sheie (11:18):
Do you understand the differences in a way that you can explain back to me?
Kristen (11:23):
I think so. You could Google it too. But in general, stage one is... What you want, you want stage zero. But stage one is that there's a tumor, it's really in one little spot, and that's all there is. So example, had mine not been on the skin, and it was just inside, it would be a one or a two, maybe just a one. I think two has to do with maybe there's more than one tumor. I may not be saying this exactly right. But it's still localized in the breast, in one spot.
Kristen (11:59):
So there's stages 3A, 3B, 3C and it all has to do with just kind of the physiology of the tumor, and then also the tumor size. So my tumor is a grade two, because it's bigger than two centimeters and under five. And then so in a grade one is under two centimeters. Mine is 2.6 centimeters, so it's not that much over. So the bottom line is that the stages really had to do with lymph nodes are key too. If lymph nodes are affected, it immediately raises the stage, I think almost automatically to a three.
Eva Sheie (12:45):
So today was your first day of chemo.
Kristen (12:48):
Mm-hmm (affirmative). But so far, I'm not puking, which is good. And I only cried once.
Eva Sheie (12:54):
What made you cry?
Kristen (12:56):
So the first thing I did was I went to have the port flushed, and then they do labs, and they make sure that they put the thing on there the little tube to do the chemo with, you know? And so like, they're the ones that access the port. And she was telling me what's going to happen, and then I think she said, "Do you have any questions?" I said, "Yeah, do I really had to do this?" And then I got tears in my eyes, and I said, "I'm sorry, it's just a lot." She was like, "I know, it's okay, we can go as slow as you want." She went and got me some water and stuff.
Kristen (13:27):
Last night, all I could think is I don't want to do this, I don't want to do this. Can't it be like it's the last day of summer vacation and then have to go to school tomorrow. But then I looked at it too as like, okay, this is the beginning of the healing. This is the beginning of the medicine, even though it's going to be a bumpy road.
Eva Sheie (13:45):
This can't beat you down, because what you've just been through is-
Kristen (13:46):
I know.
Eva Sheie (13:50):
This isn't going to be it. This is not going to be what gets you.
Kristen (13:55):
No, it can't be. No, there's no way it can be. I was talking to someone the other day about this, and I just said, you know it's almost like...even though this is life threatening, and it's cancer and everybody's like, ah, that's what you'd never want. All your life, your goal is to avoid that. But I feel like there's a roadmap, and I have professionals who have a plan... I have a team of professionals who have a plan. And with all this stuff that went on before, you know, with depression, anxiety, PTSD, like not knowing how everything was going to go, that was harder to navigate for me than this, because I didn't have any answers and got so down, and my mental state was not good at all.
Kristen (14:49):
And I had put on a bunch of weight, I was drinking a lot. Obviously, my antidepressants weren't working, and I was in a place where I like looked at a bottle of Xanax and it was like, I think this is going to be it. And then I thought about Brian, and I thought he doesn't deserve for this to be his story. That's not cool of me to do that. And I was using alcohol to numb all of the pain. And I was drinking so much.
Kristen (15:14):
When I went to rehab or treatment, however it's looked at is, there was a recipe, kind of like what I have now. They knew how to do it, and I had to do the work. But before that, it was just floundering, trying to figure it out. And so, that's a really long way around saying that this is, to me, if I do what I'm supposed to do, the chances are I'm going to be fine, and like high chances is I'm going to be fine, and other people are handling it for me, and it's going to be fine.
Kristen (15:49):
There's so much support that I have, and like so many things that are in place that it's like, I just got to show up to all of these things that they're telling me to do, and follow the directions. Nobody can do that for me.
Eva Sheie (16:03):
Well, that's kind of nice.
Kristen (16:06):
Yeah.
Eva Sheie (16:06):
What were you thinking last night when you went to bed, and then what were you thinking when you woke up this morning?
Kristen (16:10):
Last night, when I went to bed, I was thinking about I have my bag ready. Do I have all the things ready that I need to do? And I was thinking, I want to wake up and have this not be true, because that was something that like, every day when I would wake up, I'd go, oh, and I'd go oh, yeah, shit. I have cancer, I got to deal with this. Kind of like the first two months of the pandemic when I would wake up and go, "Oh, it's still here."
Kristen (16:41):
Yes, yeah. And I was concentrating on trying to get some good sleep, because I knew I needed some good rest. I got about five hours, and I woke up this morning, and you know of course, the notifications on my phone. And I was like, okay. At first, my first thought was I really was really glad I slept, and I was afraid I was going to have nightmares about it, and I didn't. I had dreams, but I didn't have any nightmares about that. It was about school. Weird.
Eva Sheie (17:13):
That'll give you nightmares.
Kristen (17:14):
The other cancer in my life. But I checked the news, and I just kind of did what I normally do and got up and took a shower. And it was this weird thing where I was like, okay, this is the last few hours you're not going to have poison in your body, and that your body will not have effects of chemo in it. And my mom had really bad effects of chemo, and so that is always in my brain.
Kristen (17:42):
And I know it was 43 years ago, and it's different, but it's always in my brain. And, so I just was like, all right, let's go. I went and I got in my friend's car, I met her and I looked at her and I said, "Are we really doing this?" Like disbelief, I think that was more than anything, this is usually a movie or someone else that you're helping or whatever, it's not you.
Kristen (18:10):
And it wasn't doom and gloom, it was more like, still shock and disbelief that this is what I'm doing, because I don't feel badly. I feel a little tired, but I don't feel sick. Well, may feel sick tomorrow, but I feel like I'm in great health. People laugh at me, I'm like, "I'm in really good health." They're like, "Are you?" I was like, "Well, aside from the obvious, yeah."
Kristen (18:36):
So, it was disbelief, and it was also a little bit of, I'm going to go kick ass. I'm very careful that I put on a pair of leggings where I have two of them, two pair, so that I never know which of them I wore to chemo first, so they're not my chemo pants. It's just those things that after the fact you think about.
Eva Sheie (18:56):
That's why I can't throw away all these ratty things that were the thing I wore to the hospital when Kari was born. I was like, none of this stuff should be in my house anymore, but I can't let it go.
Kristen (19:08):
Right. It's a profound time. And so, that's kind of what I was thinking. And really, you and I talking about this kind of invigorated me that this is going to help other people, you know, hopefully and that it was going to chronicle the journey that I feel vulnerable and open enough to just talk about, and hopefully will help somebody.
Eva Sheie (19:30):
Well, I was really surprised. You were on my mind already, because I was talking to someone yesterday morning, who's right near you, who's doing work that you're super passionate about. And all I could think about all morning was connecting you to that person because it was so perfect. And then to find out that this was what you were going through, I don't think it was a coincidence that you were on my mind yesterday.
Kristen (19:56):
No, I agree with you.
Eva Sheie (19:56):
I'm glad I caught you at the moment that I did, and that you were willing to share this story.
Kristen (20:03):
Absolutely.
Eva Sheie (20:04):
Yeah, it is going to help a lot of people.
Kristen (20:07):
Yeah. And I feel like...I don't approach things in my life from a fear perspective that much anymore, but I was scared. Last night, from about...I'm going to go from probably about four to five o'clock on last night until I went to sleep, I was scared.
Eva Sheie (20:25):
Who did you talk to last night?
Kristen (20:29):
I talked to one of my mentors here, Carrie, could be Kari. She's actually from Dallas. Anyhow, I talked to her, and we just kind of went through what was going on. And I reached out to my sister via text hoping that we could talk and she wasn't available at that point in time. Just told a couple of close friends, I'm scared, and was just reassured.
Kristen (20:53):
And I cried, I just sat here and just sobbing. And again, it was disbelief. It's weird, I'm not...I can say this, this moment, I'm not scared of the cancer, I'm scared of what the process looks like. I can only liken it to when you're pregnant, you hear about all the different things that, symptoms you could have, types of births you could have, things that could go right, things that could go wrong. Just all the different-
Eva Sheie (21:18):
Somehow people still leave out thousands of things in that.
Kristen (21:21):
Yes, yes. Completely. You just don't know how sick you're going to get if you're going to get sick. What's going to trigger you like, what smell is going to make you throw up or whatever. But that's the only thing I can kind of liken this to, because everybody's experience with chemotherapy is different. And so, I don't know what it's going to look like.
Kristen (21:43):
Part of it is I've made commitments to people in my work, and they're all wonderful, and they'll all work around me, but I feel a certain duty. You know, they're running their businesses, they have responsibilities, and they understand the situation, but I have a certain duty to let them know what's going on. So, it's also, like I have to just look at the next thing, the next action that I need to take. Because when I look at it and I go, okay, so I'm going to finish this chemo at the end of May, and then June is surgery month. And then I have a month and a half, two months to recover from that, and then radiation, and then hormones. So, I mean that's my protocol.
Kristen (22:29):
And I'm like, so that takes us to 2022. And I really built myself back up strong, and it's hard for me to consciously know I am tearing my body down in order to cure it, and then I'm going to have to build it back up. And so, I think that's what's been kind of hard. And it's not that I'm perfect, but I'm just, like I worked really hard to get to this place. And so, luckily, that's the physical body and I have my mental health and my grounding kind of in check, I feel like, this moment.
Kristen (23:09):
I don't know what it will look like in a month, but.
Eva Sheie (23:11):
I feel so grateful that your heart is where it is now.
Kristen (23:17):
Me too. Me too. I mean, that's why if there's a time to have it, and there's never a time to have it, we were talking about that, this is it.
Eva Sheie (23:26):
Exactly. So, you sent me a photo this morning of your view from your chemo chair, looking at the ocean. What was your morning like once you finally got there?
Kristen (23:40):
So once I got there, first of all, it's early so I got to pick whatever chair I wanted. Of course, I picked one that I could see the water from. And it looked over Torrey Pines golf course and into the water. That put me at ease. It was meeting with the nurse and she was telling me, like what they were going to do and she went through all the side effects and the drugs and kind of told me what to expect, you know, and gave me a big booklet. I don't know, it's probably 60, 75 pages all about chemo and about just every symptom, who to call for this and that and what to do and what to watch out for and all that.
Nurse (24:26):
We'll be getting both of these drugs intravenously through your port. [inaudible 00:24:31] Perfect. Okay. The nice thing about having the port is that it protects against extravasation, which is when the drug goes into the tissues should your IV blow for some reason. It's important with the doxorubicin because the doxorubicin is the vesicle that can cause extensive tissue damage if it was to go into the tissues, so it's a good thing that you've got that port. Here's all the side effects.
Nurse (25:00):
They're separated by the more common ones and the ones that we don't see as frequently. Like I said before, the nausea and the vomiting, we've got some medications on board for that, and then low blood counts. That's your white blood cells, your red blood cells, and platelets. So, you might see some easier bruising.
Nurse (25:21):
One of the things that we look at with the doxorubicin is how it can affect the heart. There's a lifetime dosage that someone can get of doxorubicin because it can cause heart failure and so that's why you had the echo before you came in, and will continue to do the echoes to check your heart function to make sure it doesn't drop from that baseline too much.
Nurse (25:41):
A lot of the chemo therapies have a very rare risk of developing a blood cancer after chemotherapy. Just, it works on a lot of different cells, Another serious but rare occurrence is tumor lysis syndrome. That's just when a lot of cells are being killed in your body and they start releasing electrolytes, and your body just gets really overwhelmed with it, and it can cause kidney failure. What we do to make sure that we're monitoring that is draw your labs.
Nurse (26:15):
Our restroom is actually right behind you, should you need to go to the bathroom. We just have you unplug your little friend here before you go.
Kristen (26:24):
Okay. Do I take the tube with me?
Nurse (26:26):
Yeah, you can the tube whole with you, just so it'll still be connected with the chemo. I just wanted you to know where the bathroom is, just in case.
Kristen (26:33):
Okay. Is there a taste to the chemo?
Nurse (26:38):
Um, I haven't heard anyone say that. I don't think so.
Kristen (26:41):
Good. That's good.
Nurse (26:43):
That's a really good question.
Kristen (26:44):
I'll tell you if there is.
Nurse (26:46):
Please do. That would be new.
Kristen (26:50):
So weird to feel it going in.
Nurse (26:51):
Yeah. Can you taste it? Not yet.
Kristen (26:56):
I could taste the flushing. It tastes like acetone. Yeah, I can taste that.
Nurse (27:00):
Such a pleasant taste. This that is going through the line here is the Dexamethasone, that's a steroid. What this is doing is just putting into the line, and then we've programmed the pump to deliver it over like 43 minutes. It takes like 13 minutes to get into your system, and then a half an hour, just sitting in your system and kind of like, get your body prepared before the chemo.
Nurse (27:24):
Why we do it at such a slow rate is that it can cause some burning actually in the genital area. So that's why it goes in over those 13 minutes.
Kristen (27:33):
I appreciate that. I don't want any burning.
Nurse (27:36):
Yeah. It's very uncomfortable. Not at all.
Kristen (27:40):
And then I had to sign...I had to sign that they were going to put poison in my body. I had heard how hard, how brutal the first chemo was, the one that is the red devil. Right? I can't remember the names, but it's AC Chemo if you Google it. It's the badass stuff that kills the cells. But it's also pretty brutal, especially when they nicknamed something the red devil. So, I'm thinking of it as the red devil killing the cancer cells. It's fine.
Eva Sheie (28:12):
How many other people were in the room with you?
Kristen (28:16):
There's chairs that were probably about 20 feet apart.
Eva Sheie (28:21):
Oh. Like extra COVID spacing? Is that what they were doing?
Kristen (28:24):
I don't know if it's extra COVID spacing, or if it was just like that already, because there was room for like a rounded curtain. So behind the curtain, there was a hallway, and there were a couple of other chairs back there. And there was a gentleman...I mean there were people on both sides of me. I could hear them getting their directions and all of that.
Eva Sheie (28:44):
So you couldn't see anybody else?
Kristen (28:47):
By choice. Yeah, I could have left my curtain open, but I just chose to have privacy. Maybe that's something that I know I'll feel a sense of community. But to me, today, it needed to be private, and it needed to be personal, and I needed to be able to take my selfies if I wanted to and not have people looking at me. Or, just, you know... Not that that's important, but it was, for me to... I want to see what I look like now, and in the next one. And then, like you know, I want to see a progression and understand it. Whether it's good or bad or bald or not.
Kristen (29:23):
And so, but when I got there, there were maybe three or four other patients that were being set up. By the time I left, there was a good 25 to 30. And it was the gamut of people on their phones, of people passed out sleeping. I would imagine it looked much much different before COVID, because you could have someone there with you.
Eva Sheie (29:44):
Right. You could bring a friend. Did any of that other people look really, really sick?
Kristen (29:49):
No.
Eva Sheie (29:50):
No.
Kristen (29:51):
They just look like normal people. Yeah. And like, I was feeling like this big wimp for crying because there was this guy, he had to be 90 who was there, and he's like, "Okay, I'm here." You know, he had his little bag of snacks and water and sweater, and all that kind of stuff. Everybody was just like, here's what we're doing. You know, somebody was talking about they had a mutual friend in a business and they were talking about that. Another woman when I was waiting to go in, she left and she goes, "Okay, I need to schedule my next chemo", like, you know, getting my teeth cleaned. She had all her hair, or it was a great wig, I don't know. But it was like people were just moving from appointment to appointment. Like, this is just what they were doing at this point in time.
Kristen (30:35):
There were probably some people I didn't see who were, maybe looked sicker. I didn't really see a lot of people who'd lost their hair. But it's also like, people are getting chemo. It's the oncology and hematology section of that hospital. And so, people were getting different kinds of chemo for different types of things. And so, maybe it wasn't one where they lost their hair.
Eva Sheie (30:58):
What did you do while you were there? You know, it was what, four hours long?
Kristen (31:03):
Yeah. So the pre meds before the chemo, they were two anti-nausea medications, and one was like especially for that time right there. And then the one that lasts between 12 and 24 hours, and then there was an IV steroid. And so, those three things probably took about... The education piece and getting things started, nothing really started till 9:00, medicinally.
Kristen (31:33):
And so that took about an hour. And then the red devil was 20 minutes, and then the other one was like an hour. But I had to chew on ice chips. So that's what I was doing a lot of the time, and I was reading. But because you can get mouth sores, that kind of chemo affects your whole digestive system, from literally your lips all the way out the back. And so, by keeping the ice in my mouth, it was helping to avoid the sores while the chemo was actively going in.
Eva Sheie (32:01):
Oh, boy.
Kristen (32:04):
Yeah. And so, I was listening, I was looking at the water, and it was quiet, except for the nurses and stuff because I wanted to make phone calls. But I really would have been that I would been that obnoxious person on my phone, and it would have been disruptive. I was watching everything happen. You know, I was kind of fascinated by the process, and I was reading, I was answering emails and texts and stuff like that. Just the love that came in was just so heartwarming.
Kristen (32:33):
At one point, I think I fell asleep for about 10 minutes.
Eva Sheie (32:37):
That's nice.
Kristen (32:37):
Yeah, it was weird. I was surprised I was that relaxed.
Eva Sheie (32:41):
It seems like falling asleep at the dentist. Like that would be really hard to do.
Kristen (32:46):
Yeah. Yeah. Completely. Well you know, I did kind of like...when I was a little bit nervous, I did kind of like a breathing meditation and that kind of thing. I was just really aware of what the anxiety looked like. And the steroid can get you kind of revved up, so I was trying to be aware of that. That can get you emotional. And so, what I was really trying to do is tap into where I was, and how I was feeling, so that I could be aware of when things changed, if they changed.
Eva Sheie (33:18):
And then I hope you took yourself out for lunch afterward or did something nice. Did you treat yourself today?
Kristen (33:24):
Yeah, actually, my friend Jerry, she picked me up. She dropped me off and went home for like four hours and picked me up. And, I did go back to my nanny family. And, I mean, I treated myself by playing with the baby for a few hours. Then a good friend of mine that I went to high school with who now lives in Oregon, she texted me and she said, "What's your favorite restaurant? What do you want, and I'm going to have DoorDash bring it to you tonight."
Eva Sheie (33:50):
So what did you pick?
Kristen (33:52):
I got Flower Child. I got like a sliced steak.
Eva Sheie (33:57):
There is one in the domain. I just saw it.
Kristen (34:00):
So good. You got to go.
Eva Sheie (34:01):
It's right next to Culinary Dropout.
Kristen (34:04):
Yeah.
Eva Sheie (34:05):
Now, I will try it. You know my husband would not eat at a place like that, right?
Kristen (34:09):
Well, there's steak.
Eva Sheie (34:11):
They have steak?
Kristen (34:12):
Yeah. Here's what I got. I got the steak plate... Because you can get tofu, you can get shrimp, chicken. So, I got the steak, this is my total comfort meal. Steak, mac and cheese. And the steak is like slices of like a tenderloin or something. And it's sweet potatoes, but it has like a chili sauce on it. So, yeah. It's totally carbs and red meat. Tell him to order that and he'll be happy.
Eva Sheie (34:41):
I'll just tell them they have meat and he'll be fine.
Kristen (34:43):
Okay, good.
Eva Sheie (34:44):
I mean he really goes wherever I tell him to go anyway, doesn't he?
Kristen (34:48):
Yeah, pretty much. So that's what I had. I'm supposed to eat small amounts of things. I've only really tasted the yams or the sweet potatoes because it does have a little bit of spice to it, which I love, but I did want to just try in little pieces to see what my stomach will handle. Of course, the mac and cheese went first.
Eva Sheie (35:08):
Of course.
Kristen (35:09):
I've eaten half the steak, and then probably like in another hour, I'll probably finish the rest. So, just kind of eat small.
Eva Sheie (35:18):
So what's next?
Kristen (35:20):
What's next is I have steroids to take for days two, three, and four. Those are supposed to help with side effects. And then I also have anti-nausea medicine. And so like, what's immediately next that's on my mind is just quelling these symptoms, and understanding what the fatigue looks like, for this first round.
Kristen (35:43):
And so, from what I understand, there could be a bad day, there could be four bad days. I think it also depends on what you think is a bad day. And then I think I'm okay for about a week, and feel pretty good again. Maybe a little fatigued, you know, because my blood cells are trying to replenish themselves. Oh, wait. No, wait, there's something else that's kind of cool that happens tomorrow. There is a... I can show you, let me see if you can see it. There's this little apparatus. Do you see it blinking?
Eva Sheie (36:18):
Yeah.
Kristen (36:19):
So what that is, is that this thing that they put on me today, it has a technical name, but it's basically growth factors, it injects a growth factor into you. And what that does, is that stimulates your bone marrow to produce more red cells, platelets, whatever the bone marrow produce. And this is here, so I don't have to go back to the doctor tomorrow and get another shot.
Kristen (36:44):
And, yeah. So it's weird, there is a little pinprick where a needle put a little catheter in there, and it just really felt like a pinprick. At 2:15 tomorrow, the medicine is released into my abdomen for about 45 minutes. And then about 20 minutes after that, I take it off. Actually, when the green light stops blinking... I feel kind of like Iron Man or R2D2 here with, I got the port, I got the lights, you know, and supposedly it makes a sound too. But when that's finished, the green light goes on, and that tells me it's safe to take it off.
Kristen (37:22):
So what's supposed to happen with that is your bones... I imagine it's like growing pains, you know, your bones get sore. And so of all things, what they tell you to take is a Claritin, there's something in that medication that helps alleviate the pain in your bones. Weird, I know, it's very weird. Then, along the way, tomorrow, watching what my symptoms look like, and making sure I take nausea medicine at the first, the first sign of it.
Kristen (37:51):
And I've been very well schooled on exactly how to take it, and I can alternate two medicines and all that kind of stuff. It's very weird on my phone because I had so many appointments last week to see that my next appointment is my COVID test on the 23rd, because I have to have a COVID test two days before I go in for all of this. And that's it. I do the COVID test and then the 25th, we do this all again.
Eva Sheie (38:17):
January 25th.
Kristen (38:19):
Mm-hmm (affirmative).
Eva Sheie (38:20):
Okay.
Kristen (38:22):
And between now and then, I'm getting my hair cut like Charlize Theron in Mad Max, like short.
Eva Sheie (38:30):
Were you there when she almost put her kids in Hill Country?
Kristen (38:33):
No. I didn't know that.
Eva Sheie (38:34):
I guess she came in toured the school or she sent someone with the kids to tour the school. Obviously, she didn't end up putting them in there. But that was one of those.
Kristen (38:44):
Didn't know that.
Eva Sheie (38:47):
You know, the most private public school in Texas.
Kristen (38:51):
Of course. Yeah. Of course. So, I'll have to send you a picture of the haircut that I want. Those are things that are coming up before the next appointment. I want to be sure that I-
Eva Sheie (39:00):
The hair cut.
Kristen (39:02):
Yeah, because the psychological pieces, I know, I can't manage them all, but as many as I can manage, I want to, because first of all, if my hair's long enough, I want to donate it to Locks of Love, or one of those organizations. But I could imagine it would be hard to pull hunks of hair out. And so, if my hair is shorter, maybe it won't be as traumatic.
Kristen (39:26):
And then I also want blonde tips, because my head will be white underneath when I lose my hair. And so, I want to kind of get used to what that looks like. I have little caps that I already bought because I was told you need to wear something at night to keep your head warm, which I never think about. Why would I? That's what's next.
Eva Sheie (39:50):
There's just a lot of detail to manage and I can see your sort of, um, teacher brain working through all of this.
Kristen (40:02):
Yeah, you're right. You of all people see that. Yeah. And truly, it is my way of taking control of a situation I have no control over. Because I can sit here and I can say, yeah, I see a path, and there's a recipe, and it's all going to be fine. At any point in time, it can take a turn. And I truly am not in control, but I have a plan. And so, all of these things I'm doing are my way of trying to take control, as much as I can of a disease.
Kristen (40:33):
But they're monitoring my heart. In your lifetime, you can only have a certain amount of this drug, or you will have heart failure, and I'm not going to be anywhere close to it. So, It's kind of like those things and going to appointments and just putting myself on some kind of schedule for exercise, even if I don't want to, and I'm tired, and just trying to be as normal as possible.
Kristen (40:57):
It's like, I'm fixated on this right now, but I really want to feel like I have it all on a calendar, like this lesson plan. That it's all written out, so that I can just like, okay, here's what I'm doing here, here's what I'm doing here. I have my meds in a certain area. So, again, it could go sideways at any point in time, but I'll have to get there, if that happens.
Eva Sheie (41:23):
Well, we've documented day one, I think pretty successfully here.
Kristen (41:27):
Yeah.
Eva Sheie (41:29):
And we'll come back and talk to you again, after round two, or near round two. The only other thing I want to ask you before we wrap this one up is how did you tell Brian, and how did he handle it?
Kristen (41:45):
So, that's tricky, because you know Brian, he's in New Orleans right now. He's 23, was bartending and he's really doing his own thing. He hasn't been in great contact with me. Not for any reason, except he's busy being Brian-
Eva Sheie (42:02):
He's 23.
Kristen (42:03):
Exactly, yeah. And so, my sister called him several times, and then finally left a message telling him that I had breast cancer. And she didn't want to tell him on the phone, but she wanted to talk to him, but he wouldn't answer. And that same day, I didn't realize she was doing that day, I called him and I said, there's a couple of things I really need to talk to you about, so give me a call.
Kristen (42:28):
And then didn't hear from him. And on New Year's Eve, I called him and I said, "Listen," I said, "I need to tell you, this is really serious. And there doesn't have to be any drama around it or anything like that, but I really do need you to give me a call, and I love you, and I intend on being fine. But it is serious." He texted saying, I can't call you today. I'll call you tomorrow or the next day. I love you and Happy New Year. And, I've yet to hear from him.
Kristen (42:58):
So, I did text him last night and said, please call me, you know, I have chemo. So, it's interesting, because I'm at a place right now where, you know I love my son to death, and if something again, were to go sideways, and we weren't able to see each other or something, my heart is okay with him, and I know I've done everything I possibly can. What my fear is, the demons that he's creating for him right now by some of the decisions that he may not be able to take back.
Kristen (43:34):
I'm not trying to be morbid, it's just I had to get right with myself on how did I feel, that this is about me. It's not about me when it's his journey. He's choosing his journey right now, so that I don't take it personally. Because it's super easy to take it personally, when it's your son, you know, your only child and so much of my life has always been about him and about making sure he's, he's good.
Kristen (44:01):
And, I can't take it personally. I know he loves me, I know that he's busy being 23. You know, I don't need to guilt him or anything else. I did tell him in that message, though. I said, "You know, I know the last few years I've been a lot with changes that I've made and with school stuff and all of that. And I said, I certainly hope that you never thought you had to take any of that on, and that's not who I am anymore. The drama is gone.
Kristen (44:29):
This is a little serious, but it doesn't have to be chaos. It doesn't have to be drama. And I just really want to talk to you and let you know what's going on. Because you deserve that. I just said I'm solid and I'm happy and I'm healthy except for the obvious." You know, and, maybe he just needs to wrap his head around it, just figure out how he feels.
Eva Sheie (44:50):
Thanks for listening to Breast Cancer Stories. To support Kristen, you can find us patreon.com/breastcancerstories. There's a link in the show notes with all of the resources mentioned on this episode and more info about how you can donate. If you're facing a breast cancer diagnosis and you want to tell your story on the podcast, send an email to hello@theaxis.io. I'm Eva Sheie, your host and executive producer. Production support for the show comes from Mary Ellen Clarkson and our engineer is Daniel Croeser. Breast Cancer Stories is a production of The Axis, T-H-E-A-X-I-S.io.