Defeating Stage 3 Breast Cancer: Kristen Vengler’s Courageous Battle on Cancer U Thrivers with Andrea Wilson Woods

In this episode of Cancer U Thrivers, hear Kristen’s interview with author, speaker, entrepreneur, and patient advocate Andrea Wilson Woods on her podcast Cancer U Thrivers.
Kristen walks Andrea and her audience through her experience with stage 3...
In this episode of Cancer U Thrivers, hear Kristen’s interview with author, speaker, entrepreneur, and patient advocate Andrea Wilson Woods on her podcast Cancer U Thrivers.
Kristen walks Andrea and her audience through her experience with stage 3 breast cancer, from finding her tumor in the shower, to chemo, her mastectomy and reconstruction, to radiation and beyond.
Listen to more episodes of Cancer U Thrivers
https://podcasts.apple.com/us/podcast/cancer-u-thrivers
Support the Breast Cancer Stories podcast
https://www.breastcancerstoriespodcast.com/donate
Subscribe to our newsletter here: https://breastcancerstories.substack.com/subscribe
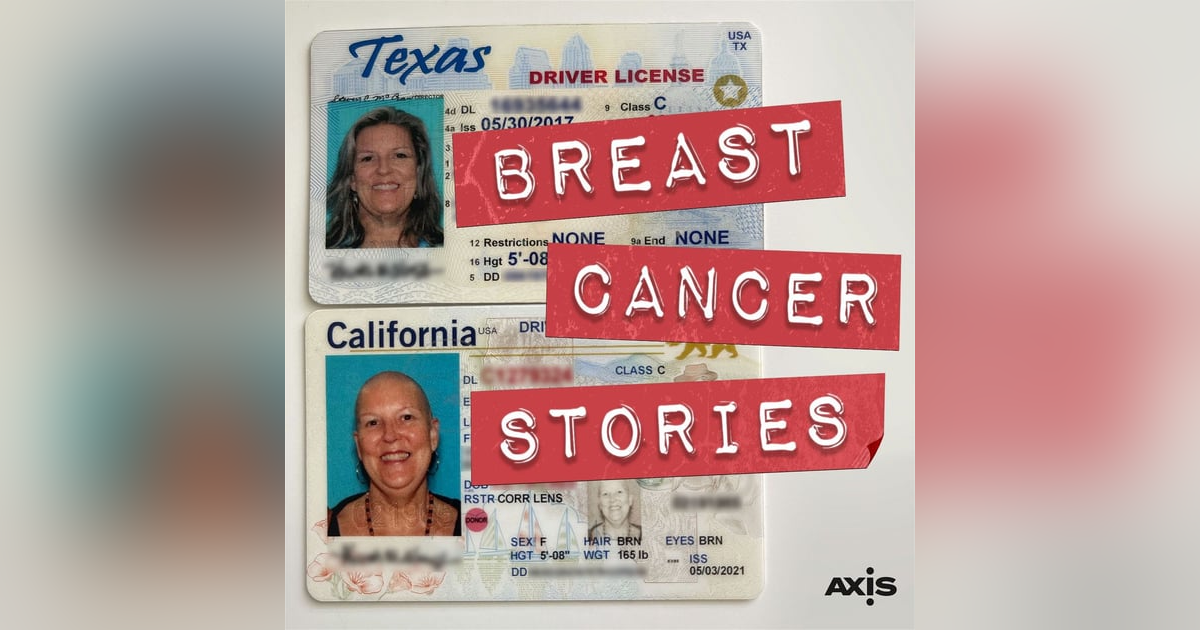
About Breast Cancer Stories
Breast Cancer Stories follows Natasha Curry, a palliative care nurse practitioner at San Francisco General Hospital, through her experience of going from being a nurse to a patient after being diagnosed with breast cancer.
Natasha was in Malawi on a Doctors Without Borders mission in 2021 when her husband of 25 years announced in a text message that he was leaving. She returned home, fell into bed for a few weeks, and eventually pulled herself together and went back to work. A few months later when she discovered an almond-sized lump in her armpit, she did everything she tells her patients not to do and dismissed it, or wrote it off as a “fat lump."
Months went by before Natasha finally got a mammogram, but radiology saw nothing in either breast. It was the armpit lump that caught their attention. Next step was an ultrasound, where the lump was clearly visible. One painful biopsy later, Natasha found out she had cancer; in one life-changing moment, the nurse became the patient.
This podcast is about what happens when you have breast cancer, told in real time.
Host and Executive Producer: Eva Sheie
Co-Host: Kristen Vengler
Editor and Audio Engineer: Daniel Croeser
Theme Music: Them Highs and Lows, Bird of Figment
Production Assistant: Mary Ellen Clarkson
Cover Art Designer: Shawn Hiatt
Assistant Producer: Hannah Burkhart
Breast Cancer Stories is a production of The Axis.
PROUDLY MADE IN AUSTIN, TEXAS
Speaker 1 (00:00):
Today's podcast guest is Kristen Vengler. Kristen talks about cancer never being done. It's one of the things she wished she had known at the beginning of her cancer journey and something she thought she would've seen with her own mother. Stay tuned for this episode.
Andrea Wilson Woods (00:22):
Kristen, thank you so much for coming on and sharing your story.
Kristen (00:27):
Oh, good morning. I am so excited to be here.
Andrea Wilson Woods (00:30):
So this is very recent for you, so you, can you take us back to the beginning? How did you even find out you had breast cancer?
Kristen (00:41):
Yeah, sure. Yeah, it's very recent. Um, so, uh, I had just relocated to San Diego from Austin, and I had been on, um, a meditation retreat. I found a beautiful spiritual community. It was 2020 the weekend, Sunday before Thanksgiving, and I was just taking a shower and all that. And, um, I noticed that my right nipple felt different than the, than the left when I was, when I was washing. Right, right. And it felt different in that it felt a little larger and it felt, um, numb, really. Like there was no feeling did it look different? And that's not a place that's usually numb. Well, um, yes. Okay. But I, but not really noticeably. So the tumor ended up being right behind the nipple. And so what had happened is that the tumor had actually come through. And the only I know <laugh>, it was well, and I, I it felt different.
(01:42)
And I, I looked down and the big thing that was different for me is there was a little bit of an indentation, like right on the ariola. Hmm. And so, and, and it was like on the bottom left. So I grabbed my camera of course, and took pictures and of both so that I could compare them and see what was different. And there was just a little, a little pink, teeny, teeny little growth, um, that looked different. And then there was this indentation. So of course, what do we do <laugh>, go to Google. Right. Diagnose ourselves. I'll always, and so, um, I looked it up and looked for pictures and all of that and said, uh, that it was likely something called PTs or Paget's Disease, which was something that was, uh, pretty serious, which was a cancer of the nipple, but it didn't necessarily mean that it, it was like a, it was a very rare kind of cancer, this PTs.
(02:44)
So of course I diagnosed myself with that and got in to see my primary care and, um, went for a mammogram and they didn't see anything, um, except they saw what was going on on the outside. And so they went ahead and did an ultrasound. Didn't find anything. I, I know. I know. So they sent me to, um, so lucky that, um, MD Anderson has a campus out here as of like five to seven years ago. And it was six miles from my house. So, um, I was referred to, um, to Dr. Rivera, my amazing surgeon, and he did a biopsy. And he's the guy who had to give me all the bad news all the time. Like, he's the nicest man. He shouldn't have to do that <laugh>. And so he did the biopsy and it came back that it was stage three, um, breast cancer.
(03:40)
And I was like stage three. I had a mammogram 18 months ago. Like a 3D mammogram. Yeah. Like how, how, you know. Um, and so like of course he, he blasted out all the referrals, you know, to the oncologist. Now, this is December 18th that I was diagnosed, so it's a week before Christmas, 2020. And I was like, you know what, you just couldn't quit 20 20 20 couldn't <laugh>. Right. Like you had to just keep giving. Right. Yeah. And so, I mean, so he, he was able to, uh, get me in to see my oncologist and a radiation oncologist and like, the whole thing. And it was this crazy labyrinth of things that places and appointments and all of that that I had to navigate. Um, and it was so fast I didn't really even have time to think about it. So, um, all we really knew is that it was, um, a stage three carcinoma.
(04:36)
And so then of course they went back and did all of the, the diagnostics and the pathology to find out exactly what we were looking at. And, um, one thing I will say is that I was a little bit like a bulldog <laugh> when I was, um, I, if they couldn't get me in for the m r i for two weeks, I was, you know, I, I wasn't rude or anything, I just said, you know what? I said I was just diagnosed with breast cancer like a week ago. Is there any way that you can get me in earlier? I am so freaked out right now and was just honest and vulnerable, you know, and that my voice probably cracked. And people really worked with me to get me in as, as soon as they could. And if they didn't have anything, they said, okay, call back at these times. Cuz this is the most likely time someone will cancel. Yeah. Or that will have something available. So, I mean, that's really it in a nutshell how, um, how I found it. And, um, I'm still a little bit terrified <laugh> that, what was the next step
Andrea Wilson Woods (05:34):
In? Did they do surgery or, and you were gonna tell us how big it was too.
Kristen (05:39):
Oh. Um, so, but in the MRI it was 2.7 centimeters, so about an inch and three quarters. Okay. And it was kind of a, an oblong mass. Um, and so the first step was, um, I met with my oncologist and she drew it out for me in record time. And it was, um, five months of chemo and then surgery. And I chose a mastectomy because I, I think PR most, the biggest reason I chose the mastectomy was probably because I could see it mm-hmm. <affirmative> and, um, feel it.
Andrea Wilson Woods (06:18):
Did you do a single bilateral mastectomy?
Kristen (06:22):
Bilateral You did Bilateral. I didn't want any breast tissue left. Mm-hmm. <affirmative>. And, um, I could have saved my left nipple and all of that, but I was, I was so freaked out that I could actually like see it. I just didn't want any breast tissue left. And because of the location of it, it would've been a, um, a unilateral for sure. Right. Because of, uh, how big it was and where it was, they weren't gonna be able to save much of the breast and it would've been just not good. Right. So, yeah. So I, um,
Andrea Wilson Woods (06:52):
What was the actual cancer? Was it a type of aino carcinoma or
Kristen (06:58):
What was it? Um, it was, um, it was stage three, um, inductive, um, IDC is what they call it. Um, uh, and it was, um, estrogen positive. Okay. Which the doctors love that because they know there's something they can do with it. Right. That, you know, there's treatment, the hormone treatment. Um, I, I've made some adjustments to, you know, my, my style of living to keep the estrogen out of my body and, and all of that stuff. And I take a, um, aromatase inhibitor, which is helps keep the estrogen out of my body because Yeah. So, um, let me go back my estrogen because I love details. Yeah, yeah. Sorry. No, no.
Andrea Wilson Woods (07:39):
So
Kristen (07:40):
<laugh>. Yeah. Yeah. You can go back.
Andrea Wilson Woods (07:41):
Why chemo? Because it's so every, as many similarities as there are, there are differences. So why was chemotherapy recommended before surgery?
Kristen (07:52):
Well, that was what, um, everybody asked me that they're like, what? Like, don't you, don't you wanna get that, that tumor out? And so, um, it was because the hope was to shrink the, shrink the, to shrink the tumor. Right. And so, really quick backstory, my mom had, um, ovarian cancer. Okay. And she had chemo, um, in a port directly into like the pelvic area. And she ended up getting rid of the cancer, but died of the effects of the chemo. Oh, that's, so after 10 years, it was a brutal situation. So chemo in my mind is like, oh, there's no way in hell no, no, just take it off. Right. And, um, in fact, I, you know, I asked her, I said, um, I don't mean to be rude cuz I know that you're the expert on this, but Well, if I'm just taking them off, then why do you want to shrink the tumor? Yeah.
Andrea Wilson Woods (08:45):
What's the point? That seems, what's the point in doing, especially doing that first.
Kristen (08:49):
Right. And what she said was, my hope is not just to get rid of your cancer for is to cure it. And while it doesn't make sense on the outside, I'm trying to, to get any micro cells that might be floating around, um, you know, in your lymph system. And that may have like breast, breast cancer cells that may have landed on your liver. You know, like little micro ones that nobody can see right now on the MRI or CAT scans or PET scans. But in five years, maybe you see, you know, a few little cancer cells growing because these micro cells were still alive. So
Andrea Wilson Woods (09:27):
I understand why chemo, but why chemo before surgery? That's the part I can't wrap my head around <laugh>.
Kristen (09:33):
I know, I know. But I didn't, I didn't, I I don't know if it was the fear that maybe the, um, or the theory that maybe the, uh, micro cells, like the longer you leave the micro cells in there untreated, the more they could grow. Okay. I didn't, I didn't really get it. In fact, um, after I left her, I think I saw her on December 30th, <laugh>, I went home and I wrote a, a note to her office through our portal that we have. Um, and I just said, you know what? I said, I understand that you're the expert on this. I said, I just think it's really, really irresponsible in the middle of a pandemic for me to be doing chemotherapy and breaking my immune system down. It's an unprecedented situation. Yeah. And I'm gonna out for the mastectomy first and copied my surgeon on it, all of that.
(10:20)
And then I started thinking about it and well, the nurse from my surgeon's office called and said, okay, Kristen, I understand I'll have Dr. Rivera give you a call next week. Um, you know, you just need to go through this in, in your way. Right. And Sunday night I realized I've probably gonna have to explain this to my surgeon and explain it to the oncologist and that they were MD Anderson professionals. And I was just sitting here in my fearful place, <laugh>, you know, questioning things. So I wrote a note back that said, um, you know, I realized that you guys have a much more extensive history of curing cancer and treating cancer than I do. So I'm gonna go ahead and go with the chemo first and I'll, you know, okay, I'll go ahead and refer to the experts. But I had to go through that process, you know, cuz I was so afraid.
(11:10)
Yeah, of course. And this was before there were any vaccines out or anything like that. And so nobody really knew what was happening with vaccines. And we knew something was coming. Right. But we weren't really sure. So, um, yeah. So that, and, and I, and I did tell her, you know, I have a, a healthy hesitation, um, about doing chemo because of my mom's situation. Yeah. And she said, I understand. And that's something that, um, that, you know, I wanna answer all your questions. I want you to be comfortable with this even though it's the most uncomfortable situation you can imagine. So see,
Andrea Wilson Woods (11:45):
That was due to five rounds of chemo.
Kristen (11:47):
I did. Well, no, five months. Five months. Sorry. Five minutes. Yes. Yeah, that's okay. How did that started on I didn't look as bad without hair as I thought I would <laugh>. Okay. I love to be honest, that's the first place you went. That's awesome. <laugh> Um, my labs, I did a lot of, um, I did a lot of work. Like I know people think this is kind of woowoo, but a lot of soul work and a lot of work on, and I had done a lot of work on trauma prior to this. Oh God. And I had a really, yeah, I had a really good, um, spiritual group and I had a just a, I really realized that this was not in my control, and so I didn't battle it. I was just like, I gotta go do this. And I was kind of a robot because I had so many appointments.
(12:38)
And so I started the chemo on January 11th, and I did, um, four rounds of what's called AC chemo. They nickname at the Red Devil. Yeah. Because, yeah. And so I had, so it was every two weeks, uh, for eight weeks. And then I did 12 weeks of, uh, Taxol. Okay. And, um, the, the last four weeks of that, there was literally a, um, what's it called? A ransomware hack throughout the healthcare system. Oh God. That's what I'm involved in here. Oh God. Right. <laugh>. I mean, to the point where they couldn't see our records to tell me how to, for them to know how much chemo to give me. Oh, my, everything was electronic. God. Well, this hap this happened in the LA it was like the last month, um, of my chemo. Wow. And, and, and, and when I was having all of my, um, consultations and pre-op appointments Right.
(13:38)
For surgery, I was meeting my plastic surgeon and he was, couldn't see anything. And so for him to figure out what he could do, and they were all taking copious notes and my heart went out to them. I could not imagine. You know, and so, uh, they actually postponed one my chemo by one week. I was up the climbing the walls. I was like, okay, May 24th has been the date in my, in my brain that I have been working toward. That's the last day of my chemo. I, right. Like, I've been working for this. That's the bell day. That's, you know, and I was upside down. Um, now that I look back at it, I'm like, oh my God, you're crazy. Yeah. <laugh>. But yeah, <laugh>, it was postponed by a week and, um, not a big deal, but it was, to me, I was, it was just, I had so focused on that date to be done it because it's just like, that's kind of in this whole journey, what, it's like you work toward little goals and you just chunk these things.
(14:36)
Right. And, and you wanna get to this and through this. And, um, I'll go back to how chemo was for me. Um, I, the first round an AC was rougher, uh, than the Taxol. Okay. Um, I was shocked. So I, um, I'm a retired teacher and my immune system was like a bull. I mean like swine flu, no big deal. Right. And so I had built my immune system over so long and within a week and a half I had three infections Oh. Of just ki just like various bacteria that we all have in our body. Right. Um, so the chemo was so I that I was really worried because from what I understand, the people, like,
Andrea Wilson Woods (15:24):
Um, well you had this experience with your mother. Right. So you had, knowing what happened to her, watching it, seeing it. Right. So I can understand that that fear, I mean
Kristen (15:35):
Three, well, three infections right
Andrea Wilson Woods (15:36):
Away is scary.
Kristen (15:38):
It was really scary. And, you know, I, um, what they tell you is that your reaction to the first round is kind of a model for the way the rest of your chemo is gonna go. I was really good at keeping ahead of the meds so I didn't wait till I was nauseous or anything like that. Smart. Um, yeah. I just, and, and I, cuz I just thought when I'd had an a c l replacement, you know, I was just, I knew I was supposed to stay ahead of the pain. Right. And so I just kind of applied that here. Um, probably for me, the worst part, um, wasn't the going wasn't the feeling poorly, it was the amount of sweating I did at night and the lack of sleep that I had. Um, I would change my pajamas three times because I would wake up just in pools of sweat.
(16:30)
Oh. Cuz my body was trying to get rid of this poison. Yeah. You know? Yeah, of course. Um, and I had, um, I, I was so lucky that I had, um, a group of people who made sure that I had food. Um, and because they said, what can we do, you know, beforehand, you know, and, and I just said, I know myself and I will be too tired and too preoccupied to eat healthy. Yeah. So I had people slicing up, uh, you know, vegetables and fruits and stuff like that and I could just combine them and That's wonderful. Amazing. Yeah. Yeah. Amazing. So that was super helpful. Um, and so I would say that was probably the worst part. And then the unknown, you know, that like, I just didn't know what was gonna happen and I was in, um, I was in action mode, you know, and so it, and I think it's because it made me feel like I had some kind of control Of course.
(17:23)
Over something that you can never have control over. Yeah. You know, and, um, and so, and I had, um, friends, um, everybody kind of took turns taking me to and from chemo, they wouldn't let me go alone. And I think it's really good cuz on those days when I was like, oh, no way, I'm going, you know, um, or do I have to really go? Um, there I was, somebody was depending on, you know, depending on me to show up someplace Right. Or that I was gonna come outta my house. And so, um, I think another huge feeling was just disbelief. As I sit here now, almost two years out from that, I still don't really believe I had breast cancer. I mean, I still, I see my breasts, my, you know, that I, they're to reconstructed that I had, don't have nipples or anything yet. And I see that every day and I still don't think I've processed all of it. Um, and that I'm never gonna be the same. Yeah. You know? Yeah. Um, and so I, and well the other thing too is it was during the pandemic, so I couldn't have anybody with me, which
Andrea Wilson Woods (18:29):
Sucks and is Yeah. Don't even get me start sucks. Yeah.
Kristen (18:34):
<laugh>. Yeah. And so, um, you know, it in, in a way, it, it gave me time to really reflect and to, um, to feel like, um, just to work through it during that time or just to relax or whatever, whatever I was supposed to do. Um, you know, to heal myself. Yeah. And my, my chemo chair was like looking at, at the Torry Pines Golf Course and over to the ocean <laugh>. And so I just <laugh> It's pretty sweet. I know there's a, yeah, there's a, there's, yeah, there's a lot, a lot worse kind of things. Yeah. And so, yeah. And so then, um,
Andrea Wilson Woods (19:08):
So let's jump to your surgery. Yeah. You Yeah. Have a bilateral, bilateral, uh, mastectomy mast. Mm-hmm. <affirmative>. Mm-hmm. <affirmative>. Sounds like you chose reconstruction. Uhhuh <affirmative>. So talk to us about the surgery and, and how that went.
Kristen (19:22):
Sure. Well, um, California opened up from the pandemic like a week before my surgery. So I was like, oh my gosh, that means I can have somebody with me cuz you know, right. It's so important. Hmm. Well, it didn't get to happen. Um, and so that was, that was a hard piece. Um, I also, the, the place that, that they did the surgery was at Scripps, um, green Hospital. Um, it's an ambulatory surgery, uh, uh, surgery center, which I didn't understand what that was, where you would like literally walk into your own surgery. And that was interesting because I thought I would be wheeled in and just, you know, um, so I was, I was ushered into the room, um, and, you know, um, sat in a recliner and the nurse got me ready and all of that. And my plastic surgeon, Dr. Patella and my oncology surgeon, Dr.
(20:13)
Rivera, who were both incredible human beings as well as like top of their, top of their game professionally. Um, they came in and drew the lines and it was really cool to see them collaboratively working. Um, so Dr. Patella was drawing the lines and Dr. Rivera was, was helping to figure out, you know, where he, how had a, it was a skin saving mastectomy, so they, I knew that the nipples were being removed and all of that. Um, and so it went really well. Um, I didn't, the only thing I really had a hard time with is, um, I was in an incredible amount of pain for about two hours afterward, and it's just, um, it, it went away afterward. Yeah. You know, but I woke up in, in incredible pain. And so it just, I, I know everybody has different pain thresholds and responses to pain and all of that.
(21:05)
So that was just mine. And it's kind of a fog, I think. Um, I'm grateful for it. And on purpose. Um, the first, I was there for two nights, um, and I remember people coming in and out and all of that. Um, and I will never forget the, this moment. My, um, oncology surgeon, Dr. Rivera came in and he said, um, I really need you to hear me. And I said, okay. And he said, um, this isn't the outcome we wanted. And I, what? And he said, behind it, he, yeah. So he is behind a mask and I, so I can't see his whole expressions or anything. And he said, um, we did, uh, they did something called a sentinel, a sentinel, uh, biopsy, sentinel node biopsy. Which means that they, um, during the actual surgery, they actually inject some radioactive dye into the tumor to see where it, which lymph nodes it goes to first.
(22:02)
Right. And then they, they take that lymph node and they biopsy it right there. And so he said, um, the lymph node that we biopsied, um, did show cancer. And I said, okay. And he said, so we, um, we took, I don't, he, he doesn't even know how many nodes he took at that point in time, cuz it's hard to know. He said, um, when the pathology gets back, I will get, you know, I'll call you, we'll talk about it. And he was very compassionate, you know, um, with it. Um, but he said, I, I, I just, I need you to sit with that. You know, we were really hoping there was no lymph node involvement. Right. That doesn't mean it's the end of everything. It just means this isn't the ideal outcome. Right. And you may as well have told me that I had stage four pancreatic cancer, brain cancer, all of the things together because, um, of course I didn't dig into this with breast cancer.
(22:56)
I knew everything there was to know about ovarian cancer. Right. And that I spent my whole life avoiding ovarian cancer. Right. Never thinking about the breast cancer. And so, um, he, uh, so I sat there and, and I was just like, oh, stage three lymph node involvement, um, history, you know, um, this is gonna be a rough couple years. And I that's wrong. Anybody who's listening to that, I was so, um, uneducated, and I don't mean it's in a negative way, but truly ignorant to what that really, really meant, you know? And so then, um, I, I went home after a couple days and was in a lot of pain, but stayed ahead of the pain, you know, with the pain meds and all of that, and was not re I didn't really realize that it was true that I would be like a, um, uh, what's the dinosaur? Um, is it tactile that has the short arms? Uh, you know what I'm talking terrex about T-Rex. That's it. Yeah. T-rex a T-Rex. Because I couldn't move my arms, um, because of, you know, where the like, because they, they took so much breast tissue, um, and I mean, it was like, everything was just, it was wrapped. It was, um, did you have tissue? It was exactly what they told me. Oh, sorry. Yes. Yes. They put in, they put tissue expanders in. Um, and that wasn't super comfortable. I was
Andrea Wilson Woods (24:22):
Gonna ask, was that
Kristen (24:23):
Painful <laugh>? Mm-hmm. <affirmative>? Um, I don't know. And I never asked, but it felt like, so the tissue expander for anybody who doesn't know is basically it's a placeholder for your, um, for your implants. Right. And we knew pretty early on that radiation was on the program. You did. Okay. And so my mm-hmm. <affirmative>. And so my plastic surgeon, um, allowed for that. So he's worked very closely, um, with, I mean, it really felt to me like the, the tissue expander that is flat on the bottom. It's like a, it's like a half a grapefruit, basically. Okay. All right. Um, and, and the tissue expand on the bottom part. I feel like it was stitched into my chest wall because if I moved it was excruciating. That was the worst pain. Probably was like, try. Yeah, I bet. I bet it was, you know, um, and just trying to get into a position where I could get up.
(25:15)
I actually had a step stool to get into bed, and I'm a side sleeper, so I had to learn how to sleep on my back. Oh, God. And so I had a wedge and all kinds of pillows and every, I called it my pillow throne because I literally, it was like, I built a recliner into my bed. Nice. <laugh>. I love it. Yeah. I like it. I didn't even think I could go get a recliner, you know, but I built it into my bed. And so, um, it was super important to have my arms, um, elevated. Yeah. So they, so there wasn't a lot of pulling also. So, um, the recovery on that was exactly what they said it would be. Um, I, what they were doing is that they were injecting saline periodically into the, uh, expanders to, um, and they were over the muscle, um, to make the, to make room for the implants. And they had to expand the right one, like twice as big as the left, because radiation sh pulls the skin up and shrinks 'em. And so, um, it was very weird. So you're having
Andrea Wilson Woods (26:19):
Radiation while you were getting these tissue expanders? Getting the saline. This was all mm-hmm. <affirmative>. So
Kristen (26:24):
This was, this was all, this was
Andrea Wilson Woods (26:25):
Your summer of 2021, is what you're telling me,
Kristen (26:28):
<laugh>. Yeah. It wasn't, it wasn't great, I'll be honest. <laugh>. Yeah. So it was, um, I, I think I saw, I think the first, uh, fill was, and that's, that's done by the plastic surgeon, um, with maybe two weeks afterward. And I had, remember this one day I had, um, a meeting with my oncologist for the first time after the surgery and after the pathology was done, I'd had a, a, I just had a meeting with Dr. Rivera about the pathology. And then later that day I was going to meet with the radiation oncologist. And I was just like, it was just ba it was too much. Yeah. Like, I was like, on complete overdrive. My nervous system was thrashed. Um, but, um, how much radiation did you have? Uhoh? Too much <laugh>. I <laugh>. That's a, that's okay. Well, I didn't realize. So everybody always said radiation was the easiest part.
(27:27)
Right. If you've had chemo, you can, that depends. I'm still thinking. Right. It's different for everyone. So a lot of people, they have like a zap and then they're done. Like, it takes 'em longer to get positioned for the, the beams to, to hit the right places. Um, and they were done in 15 minutes. Like it took 'em longer to park. Mine was 45 minutes. I had eight spots that they radiated. Wow. And yeah. And it was, um, and it's not normal. Like, that's not what normally happens. But because my lymph nodes were so deep, um, my radiation oncologist explained to me that, um, that she would rather damage my skin than my heart. And I was like, okay, cool. I really appreciate that <laugh>. That's, you know, we can fix the skin. Yeah. Um, but the heart you can't. And so, um, there were just so many, they really wanted to get the lymph nodes.
(28:22)
Yeah. And so I'll back up and give you good news. That one lymph node he took was the only one with cancer. Oh, that is good news. All the, the, the other 10, cuz he took 11, it turned out with the pathology. Um, the other 10 had no, no, um, signs of cancer. And we also figured out that the chemo had very little effect. There was a little bit of scarring on the tumor, teeny bit like a cent, like a millimeter on one side. Um, and it had no effect on the lymph nodes. And so I was, I, that was a really hard piece for me to digest because I had, I had probably put on 40 pounds through the, um, just all the, all the treatment, all of the, um, the swelling, all of the steroids. And prior to that, I had lost 65 pounds and was in the best shape of my life when I found my tumor.
(29:16)
And it was just rude. <laugh> <laugh>. It was rude. It was rude. And so, um, so that was that I really had to just, I had to really embrace that all these micro cells that were floating around were gone. Yeah. I had to really see that as, as the, the silver lining. And we also found out that the tumor wasn't 2.7 centimeters, it was three and a half. And so I don't know if it grew during that time. I don't, and MRIs can be inaccurate. I mean, they're obviously not seeing it firsthand. Right. You know, um, and that, you know, I really did need radiation and they, they wanted to, because I had lymph node involvement, they really wanted to get all of, you know, all of the spots. So it was any, it was from like, um, it was a quadrant from like below my, maybe a little bit below my chin or mid throat, um, all the way over to my shoulder and then down around back and back up through the middle of my chest. And um, how
Andrea Wilson Woods (30:22):
Many radiation treatments did you have?
Kristen (30:26):
Uh, 32. So it was six weeks. When I say I got the full MD Anderson experience, like I don't think there was much that I missed <laugh>, I don't <laugh>. I got the six weeks of chemo checking the
Andrea Wilson Woods (30:39):
Boxes. Okay. That's really
Kristen (30:40):
Fun. Oh yeah. And so, but the good piece to that, and it, here's Pollyanna on this, you know, is that anybody who is going through this, I can help them because I've been through the majority of it now. I was estrogen positive. There are all kinds of different variations of breast cancer. And what's really interesting about it is it kind of unravels or kind of, uh, what's a better word is um, it exposes itself a little like along the way. So first you find out that you have cancer, then you find out at stage three, then, you know, you find out more and more and more. And there's never a dull day. There's, you know, you never, there's always something going on. And so I had really extreme burns from the radiation and, um, to the point where they gave me the same medication, uh, for the radiation burns as they did for, um, after my mastectomy. Wow. Uh, cuz I couldn't, yeah. It was, it was pretty bad. So, um, but you know, I just look at it and I'm like, I got through that. Yeah. You know, and it was all really fast. I mean, within nine months. Okay. I had gone through all of that. When
Andrea Wilson Woods (31:52):
Did you have the reconstruction?
Kristen (31:54):
The reconstruction was June 22nd.
Andrea Wilson Woods (31:56):
Okay. So pretty soon after radiation it was mm-hmm.
Kristen (32:00):
<affirmative>? Oh no. The, it was after, right after chemo. Yeah. Okay. So what I realized is that there's a sweet spot. Dr. Rivera told me a sweet spot for the surgery between, um, two weeks after and 30 days, um, that if it goes past 30 days, he, you know, he, it it's, it's problematic for him. And before two weeks your immune system isn't ready for it yet.
Andrea Wilson Woods (32:22):
So wait, did you have, and so I've just, I'm trying to like get the timeline. So did you have the reconstruction before or after radiation?
Kristen (32:29):
Before, before. Before. So, yeah. So it was chemo from, um, July 11th to June 2nd. The mastectomy and reconstruction was on, um, June 22nd. And I began radiation, uh, the beginning of August. Okay. And, and finished at the end of, uh, September. And how are you doing today? I'm doing really well. Um, I had, uh, two more reconstruction surgeries and so they did a, they did the implant exchange this past March. And then, uh, they did a fat transfer, um, to, uh, make it more rounded to make the, the breast more rounded. So it didn't just look like I had my chest and then a half a grapefruit on it. Right. So it, it had, you know, so anyway, um, I'm doing well. The, um, the biggest problem that I still have, um, is the results from chemo. And, um, I had really horrible neuropathy, um, about a year ago right now.
(33:32)
It started in my feet. Oh. And to the place where I was falling down, like literally like falling. Um, and so I had to kind of watch that. So the neuropathy cleared up, but what happened is the fascia in my feet and ankles just was bound. And I lost structure in my feet because of it. And, um mm-hmm. <affirmative>, what is that? And so I had like, my arches fell it just like my, my foot when I went to a sports, uh, sports physical therapist, he just said, your foot just kind of dangles. I mean it, if there weren't bones, it's just kind of dangling there. Wow. And it doesn't, yeah. So all the, all the muscles, all of that stuff were kind of messed up. And because the fascia was so bound, I had <laugh>, this is ridiculous. I had strained achilles tendons. Oh gee.
(34:19)
And so, oh God. Because if you think about it, it's, everything's pulling down. Right. And so all your muscles are super tight. And so, um, I got some special arches and, and all of that. And I, um, I mean, I'm not trying to be dramatic, but I actually have a handicap placard Yeah. Because it's so painful to walk from. Sure. You know, place to place. But the sports therapist really helped me to get, uh, rid of the, the plantar fasciitis and all of that. And I just have, I think I have a, a routine that's about two to three hours a day of stretching and exercises to strengthen everything and to keep my, you know, and massage stuff, like a massage gun thing and all that. So that's, I mean, that's the biggest residual piece aside from my obvious brain fog <laugh>. And it's, it's <laugh>.
(35:08)
Um, I'm gonna, I'm blaming the brain fog forever. I don't care if I'm 85 with dementia. It's the brain fog from chemo <laugh>. Um, and, but you know, I, um, I'm healthy. I went, I saw my oncologist and, um, Dr. Ali and Dr. Rivera, the surgeon, uh, about two weeks apart in August. And they both said, you are really healthy right now, Kristen. Oh, that's great. You are really healthy. So that's crazy. I had a scan. It's such great news. Um, I had a scan last march, um, and it was, cause I had a little bit of a scare and it was perfect. Oh, that's great. So yeah, it's, so, you know, I'm gonna attribute that to positivity and to, um, my incredible medical team.
Andrea Wilson Woods (35:53):
Kristen, let me ask you. Yeah. What is one thing you wish you had known at the very beginning of your cancer journey? Because you came into this as some, with some experience with your mom mm-hmm. <affirmative>. Um, but what about you? What, what do you wish you had known?
Kristen (36:10):
Um, I should have seen it with my mom especially, but I didn't. Um, the cancer doesn't go away. That it's not like having an a c l surgery where you do all the things they tell you and then it's better or it's 95% better. Right. Um, and I'm not trying to be gloom and dome, but you know, we're cancer free till we're not. And that's, that was, it was put that way by my surgeon. And he, he has ca he, he had cancer. He's in remission from cancer, so he can talk, he can speak that language. And so I wish I would've known, um, that when you're outta chemo, you can still have problems from it a year later, you know, um, that it doesn't really, you're never the same. Yeah, yeah. Yeah. Uh, and, and you see things for, in a different way. Um, yeah.
(37:08)
That, I mean the, the, and, and I'm not trying to be negative about it, you know, I, I feel like, again, I'm still surprised I had cancer <laugh>, you know? Um, and that I'm a breast cancer survivor now hour, whatever, however people wanna talk about that. Um, that's, you know, it, it's something that always is. Um, I don't live with a fear of recurrence. I live with a respect Oh, love that I don't take care of myself. Mm-hmm. <affirmative>, I love that, like respect that it's, it's a, it's a respect that, you know, I gotta stay on my game. Yeah. But if it were to recur, that doesn't mean I did anything wrong. You know? Of course. Of course. Because a lot of people think course not. No, I know. But a lot of people think, what did you do to get cancer? You must have been obese. You must have been unhealthy. You must have been, you know, like, um, and there's people who get lung cancer who never smoke. Of course. So, you know, so, um, yeah. That's, that's probably the, the, the thing I, you know. Yeah.
Andrea Wilson Woods (38:08):
Okay. And if you could only do one thing to improve healthcare in the US what would it be and why?
Kristen (38:15):
Well, um, I know there are a lot of arenas where things need to be changed. I know. And you get one <laugh>. I know. Dang it. Um, and this is something I feel pretty passionate about, is that, um, I was diagnosed, I had dense breasts. Right. And I would, I guess the one thing I would do is make MRIs standard for people who have dense breasts, who have certain, certain criteria. Cuz mammograms are gonna find a lot of it. But there are, um, and a lot of, a lot of people think that if they don't have a history of it, that they don't have to worry about it. Or maybe they can skip their mammograms or something. And that's not, it's not true. Only about 10 to 15 people with breast cancer have a history in their family. Right. And so, yeah. So, um, you know, I would say find, find a way to, I don't wanna say standardize, but not make it a grueling procedure or an out-of-pocket expense Yeah. To get an M mri. Cuz to me, I had a mammogram that, an ultrasound, that another mammogram. Right. And so I'm betting that the cost of that is probably the same as the mri. Yeah. You know, and so, I mean, I, that's what I would do that Okay. And, and make it have it covered by insurance. And that's, and because that's, it's, it's personal, you know? Yeah. I love the specificity of that.